Recent Comments
No comments to show.
Introduction:
Achilles tendon injuries are common among runners and can significantly impact their ability to run. As a physiotherapist, it is essential to guide individuals through the recovery process and help them determine when it is safe to resume running. In this blog, we will discuss how to assess your readiness to return to running after an Achilles tendon injury and provide a structured approach to minimize the risk of re-injury.
1. Listen to Your Body:
The first key to determining when to start running again is to listen to your body. As you recover, pay attention to any pain, discomfort, or swelling in the Achilles tendon area. Gradually introduce activities that don’t aggravate your symptoms, such as walking or biking, and monitor your response. If your symptoms worsen, it’s a sign that you need more time to heal.
2. Consult with a Physiotherapist:
Seeking professional advice from a qualified physiotherapist is vital in establishing a personalized rehabilitation plan. They will assess your injury, consider your individual circumstances, and help you develop a safe and effective progression towards running. Physiotherapists also use specific tests, such as the single-leg heel raise, to determine your Achilles tendon strength and readiness for running.
3. Maintain Flexibility and Strength:
Building up strength and flexibility in the lower leg and ankle is crucial for a successful return to running. Your physiotherapist will prescribe exercises that target the Achilles tendon, calf muscles, and surrounding ligaments. These exercises may include calf raises, eccentric heel drops, towel curls, and calf stretches. Consistency and regular progression are key, avoiding overloading the tendon too soon.
4. Gradual Return to Running:
Returning to running involves a gradual and systematic progression. Following your physiotherapist’s guidance, start with a walk-run program, incorporating short bouts of gentle running interspersed with walking breaks. Begin with a slow pace, soft surfaces, and reduced frequency, gradually increasing the running intervals over time. Ensure you have adequate rest days between running sessions to allow for recovery.
5. Monitor for Warning Signs:
Pay close attention to any warning signs during your return to running phase. Excessive soreness, swelling, sharp pain, or a sudden increase in discomfort are signs that you may be pushing too hard or too fast. Adjust your training accordingly, and if necessary, consult your physiotherapist for further guidance or evaluation.
6. Consider Cross-training:
To aid in your recovery and reduce the risk of reinjury, consider incorporating
cross-training activities, such as swimming, cycling, or strength training, into your routine. These activities help maintain cardiovascular fitness and overall strength while reducing constant stress on the Achilles tendon.
Conclusion:
Starting to run again after an Achilles tendon injury requires patience, proper rehabilitation, and careful monitoring of your progress. It is essential to work closely with a qualified physiotherapist who can tailor your recovery plan to your specific needs. Remember, the goal is not just to resume running but to do so safely and without risking further damage. By following these guidelines and listening to your body, you can gradually return to the activities you love while minimizing the risk of future Achilles tendon issues.
Consult your physiotherapist at 4053 6222
What is abdominal muscle separation or Diastasis of the Rectus Abdominus Muscle (DRAM)?
Abdominal muscle separation is when the two long muscles called the rectus abdominus muscles separate from each other during pregnancy. This is the body’s common and NORMAL safety mechanism which occurs most often in the second and third trimester of pregnancy as the body changes to make room for the growing baby.
What this means for you postnatally?
This separation will usually resolve in the first 6-8 weeks postnatally and is usually only considered to be a concern if you are still feeling the muscle weakness/separation after this period of time. Up to 1 in 3 women will still experience some separation a year after the birth. The depth/width of the muscle separation are the most important components in assessing this potential concern and needs to be done by a physiotherapist or doctor.
Why is this important?
If the muscles remain separated with a significant depth it means the deeper stability muscles aren’t providing your back with the full support it requires. The other structures in your back (vertebrae, disc, ligaments) then have to compensate for this weakness and this may also increase in the incidence of lower back pain.
What can be done to help?
• Exercises to strengthen the deep abdominal muscles.
• Wear an abdominal support, such as Tubigrip or high wasted compression underwear/tights
· Avoid sit-ups or abdominal crunches until you have seen your physiotherapist
• Getting in and out of bed with the log roll- Sit on the edge on your bed and then lean onto your elbow and at the same time lift both legs onto the bed. From this position, you can roll onto your back. For getting out of bed it is the opposite.
• Minimise lifting anything heavier than your baby or anything that causes your tummy to bulge with strain.
How do you monitor the recovery of your Abdominal Muscle Separation?
• Lie on your back with your knees bent and place your fingertips across your belly at the level of your belly button.
• Lift your head and shoulders away from the floor (a small sit up) and feel for the sides of your abdominal muscles coming together.
• If you can feel a gap wider than one finger then you may still have a separation
Exercises to start before your Six Week Postnatal Physiotherapist Assessment:
• Pelvic floor exercises (see blog “The Physiotherapist wants to see me at six weeks post-natal, what can I do before this to help my recovery?” for more information)
• Deep abdominal strengthening exercises:
o Lie on your back with your knees bent and your feet flat on the floor.
o Place your hands on your lower tummy just inside your hip bones.
o Gently tighten your tummy muscles, pulling your belly button in towards your spine.
o You should feel your back flatted on to the floor.
o Do not hold your breath.
o Hold this contraction for 10s. Relax and repeat 10 times.
o Repeat this up to three times a day
What else will the physiotherapist assess at your six week postnatal review?
• Will check any scarring (caesarean or vaginal)
• Will check and correct your posture breastfeeding/baby holding or carrying
• Address any continence concerns
• Mobility assessments
• Musculoskeletal assessment
• Rectus abdominal assessment for any separation
• An optional pelvic floor check (either internal or external, whatever if preferred if safe to complete).
• Give you advice on resuming sexual intercourse safely
• Give you advice on good bladder and bowel habits
• Return to exercise advice and individually tailored exercise program to work towards your goals
Contact Proactive Physiotherapy today and organise your six-week postnatal appointment with one of our Pelvic Physiotherapists on 07 4084 0602.
References:
Department of Health and Aged Care, Australian Government. (2022). Abdominal separation (diastasis recti) https://www.pregnancybirthbaby.org.au/abdominal-separation
The Royal Women’s Hospital, Victoria Australia. (2018). https://thewomens.r.worldssl.net/images/uploads/fact-sheets/Abdominal-muscle-seperation-270719.pdf
As
healthcare professionals we all deal with patients with chronic pain every day.
According to the Australian Institute of Health and Welfare, 1 in 5 Australians
over the age of 45 suffers from chronic pain. In my practice as a physio, I see
young people also suffering from chronic pain on a daily basis.
Chronic pain can result from injury, surgery,
musculoskeletal conditions such as arthritis, or other medical conditions such
as cancer, endometriosis, or migraines. The term “chronic pain” refers to pain,
persisting longer than 3 months from different diagnoses and epidemiology.
Pain that is acute, or short-term, is a response to damaged
tissue and usually disappears once the tissue has healed.
Chronic pain is much more complex!
Consider the Biopsychosocial model of chronic pain:
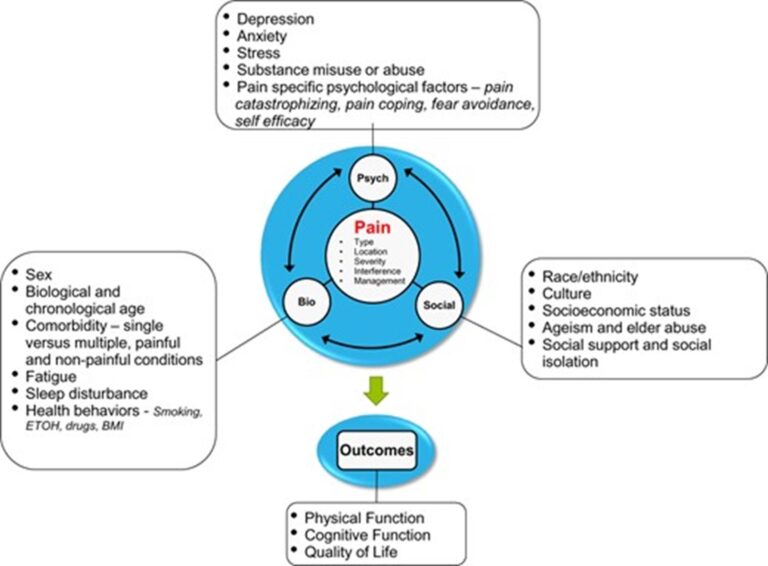
Image source: https://www.physio-pedia.com/Biopsychosocial_Mode
So, chronic pain may result from damage to body tissue from an acute or chronic condition.
But changes in the nerves or nervous system that result in the nerves continuing to signal pain after the original condition has healed (Painaustralia 2019a).
There also may be no apparent physical cause (Treede et al. 2015; Painaustralia 2019a).
Thus, attitudes towards pain and biological changes in the perception of pain may influence the experience of pain. (Molton & Terrill 2014).
There has been many studies and research to try to understand people’s experience of pain. One thing is for certain: Pain and the experience of pain is subjective. For instance, according to Professor Lorimer Moseley, of the USA in Adelaide, the more pain we feel the less life threatening it is. Why is this?
However, people suffering from chronic/persistent pain do have a lower life expectancy: It can disrupt nearly all aspects of someone’s life – beyond physical pain, it can impede their ability to work and participate in social and other activities like they used to. It impacts their relationships and cause feelings of isolation, frustration, and anxiety. Recently, Australian researchers have found that there are actual physical alterations happening in a patient’s brain that likely leads to negative changes in their personality.
Chronic pain itself is not life-threatening, but it leads to higher rates of depression, suicide, and opioid use.
What can we do about it?
As physiotherapists, we have many ways of trying to understand a person’s level of perceived pain, which is especially important for us to know if and how our treatment made a difference.
How can we address the changes in the nerves or nervous system, attitudes towards pain and perceived pain?
By combining an active and passive approach to meet the patient where they are at.
An active approach:
1) Empower the patient to understand their condition.
2) Provide education regarding chronic pain.
3) An exercise program that is gentle, gradually challenging fear and enhancing a sense of achievement.
4) Create an understanding, acceptive space to promote confidence.
5) Home exercises to promote self-management.
6) Self-management techniques to cope with setbacks or flare-ups.
7) Adopt a coaching role, assisting the patient to problem solve, rather than a traditional treatment plan.
A passive approach:
1) Hands-on modalities, including different massage techniques, joint mobilisations, myofascial release, and craniosacral therapy.
2) Electrotherapeutic modalities and cold/heat therapy and vibrations.
3) Acupuncture/ Dry Needling
In my experience, a combination of an active and passive approach is more appropriate and most useful.
To summarise:
An image to explain chronic pain:
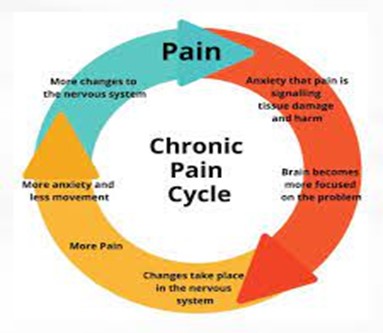
Our role as allied health professionals is to intercede into
this pain cycle and interrupt it. As we know, each person’s pain – experience
and perception are different.
So, we need to work with what the patient allows us to work
with. We need to do this with the patient, not “to” the chronic pain patient.
We need to have compassion, create trust, and provide
excellent care.
Resources:
www.aihw.gov.au
https://www.iasp-pain.org/publications/relief-news/article/pain-revolution-lorimer-moseley
https://www.healthdirect.gov.au/chronic-pain
https://www.adelaide.edu.au/painresearch
https://my.clevelandclinic.org/health/diseases
Many times, dizziness and vertigo are used interchangeably. However, the two are quite distinct with vertigo relating to a sensation of the environment moving or spinning. On the other hand, dizziness is a sensation of light-headedness, feeling faint and woozy, and unsteady with loss of balance.
Vertigo
Vertigo is a symptom of a range of conditions, so it is important to share your detailed health history.
Benign
Paroxysmal Positional Vertigo (BPPV) is the most common type. Although not fully understood, BPPV is thought to arise due to the displacement of otoconia (small crystals of calcium carbonate) from the inner ear into the fluid-filled semicircular canals. These semicircular canals are sensitive to gravity and changes in head position can be a trigger for BPPV.
Benign= not harmful
Paroxysmal= sudden onset
Positional= positionally triggered
Vertigo= sense of the world moving.
Triggers
The vertigo may be triggered by tilting the head, rolling over in bed, looking up/under and sudden head motions.
How is BPPV assessed?
The inner ear is responsible for keeping your eyes steady during head movement. The tests use will assess (Nystagmus) involuntary repetitive eye movement in response to head movements as well as the vertigo. Nystagmus can present with different eye movement directions in different clinical tests. This leads to the diagnosis and correct identification of the canal affected in BPPV
Management of BPPV
There are some techniques that can be used to reposition the crystals, dependent on the canal in which they are. The most commonly used technique is the called the Epley manoeuvre, however, there are other effective methods that can be used depending on individual findings during the assessment. You will be given advice on
life-style changes such as avoiding lying on the side that tends to trigger the vertigo.
If you need a further support, please contact Proactive Physiotherapy 07 4053 6222
As we now know, as we age, our spines changes :
Our discs dry out and provide less vertebrae cushioning. They also become more vulnerable to herniation.
The ligaments and muscles in our spine become less flexible.
Our spine joints lose fluid and cartilage, contributing to spinal osteoarthritis.
Our vertebrae lose mineral density and become thinner.
Although no living thing on earth gets any younger, there are a few things we can do to help lessen or, at least, postpone and maybe prevent these normal ageing changes:
The best tips I can give is the following:
Gentle stretches of the lower back, hips, and buttocks are always good at maintaining flexibility. Aquatics, yoga, and Pilates are all very good forms of exercise for the spine.
Any excess weight puts stress on all our joints, especially the lower back.
This means that there is a right way and a wrong way of using our backs daily. With activities like lifting, pushing, pulling, carrying, picking up and cleaning, there is a certain alignment and movement pattern that we need to use to take care of our backs.
In our day-to-day living, we may not be moving like our bodies like to. We sit at desks, use computers, laptops and cell phones. When home, we watch TV… Our spines like movement. Prolonged sedentary positions weaken our muscles and make us prone to injury.
This is of the utmost importance for a healthy spine. Standing or sitting crookedly, especially in a work environment, aggravates tension in certain areas and can strain joints.
Regarding all these things mentioned – we can help you! If you need any education. Advice and assistance – call your physio. We want to work with you to take care of your spine.
Call us 07 4053 6222 for an appointment to let us teach you how to take care of your spine.
Giving birth can be an exciting and overwhelming time and leave you with questions about your postnatal recovery. Generally, it is six weeks before your doctor and/or physiotherapist will see for your review to answer your questions and address concerns.
To help with the time in between, we have put together some handy tips to get your recovery started before you see your professional for your six-week review.
Ice & compression:
Guidelines for lifting:
Supportive positions:
Good bladder and bowel habits:
The best toilet position to avoid straining:
Exercises to start:
At your Pelvic Health six weekly Postnatal Review
Contact Proactive Physiotherapy today and organise your six-week postnatal appointment with one of our Pelvic Physiotherapists on 07 4084 0602.
ITB or Iliotibial Band Syndrome is a common injury among runners and athletes that causes pain and discomfort in the knee. The ITB is a thick band of fasciae that runs from the hip bone to the knee and helps stabilise and support the leg during physical activity. When the ITB becomes tight or irritated, it can rub against the bone and cause inflammation and pain in the outer part of the knee.
There are several factors that can contribute to the development of ITB
syndrome, including overuse, improper training techniques, and biomechanical abnormalities. Runners with high or flat arches, tight hips or hamstrings, and weak gluteal muscles are more prone to developing knee pain due to ITB syndrome.
To manage ITB and knee pain, it is essential to identify the underlying cause of the injury. Rest, ice, and stretching exercises can help alleviate pain and inflammation. Physical therapy may also be recommended to strengthen the muscles around the knee and glut area and improve flexibility.
Prevention is key in avoiding future ITB syndrome flare-ups. Runners can minimise their risk by gradually increasing their mileage, maintaining proper form, and using proper footwear. Stretching and foam rolling exercises that target the ITB and surrounding muscles can also help prevent tightness and inflammation.
In conclusion, ITB syndrome is a common injury that can cause knee pain in athletes and runners. Understanding the causes of ITB syndrome and taking preventative steps to manage the injury can help athletes continue to train and compete without discomfort or pain.
nIf you think you have ITB, please contact your physio, 07 4084 0602 for an assessment.
Many of us have had the experience of yawning and feeling the jaw joint pop from overextension, but is it normal for the jaw joint to click, pop or grind when chewing and talking? The short answer is no. When the jaw functions properly, it will open and close smoothly and quietly. It will also feel comfortable to eat just about anything on the menu.
When the jaw joint starts to act up – making sounds or causing pain – it can mean that something is not functioning the way it should. At Proactive Physiotherapy clinic, our physios examine jaw function to ensure that patients remain comfortable whether yawning, laughing or enjoying a meal with friends.
Jaw health is part of overall dental health and being able to chew food like crunchy vegetables can help with whole-body wellness. So, if you have noticed that you avoid certain foods because it’s hard on your jaw, we welcome you to come in for a jaw assessment.
What Causes Jaws to Lock or Click?
Sometimes, jaw dysfunction, called TMD (temporomandibular joint dysfunction), occurs due to trauma such as an auto or sporting accident. Other times, the cause could be more subtle – like the bite not coming together correctly or misaligned teeth or perhaps even issues in the upper cervical spine.
Other signs can include:
Do You Have Headaches or Jaw Pain?
Our compassionate physio team may be able to provide relief for some of the most common symptoms associated with jaw pain. We welcome you to call 07 4053 6222 to arrange an appointment and get the relief you need.
The pain may radiate into the forearm and wrist. The pain usually comes on gradually, and is made worse by repetitive extension of the wrist as when making a fist, shaking hands, carrying bags/ groceries, lifting saucepans, turning on taps or using pliers.
Tennis elbow often lasts for several months, but physiotherapy treatment will be able to help to use current evidence based management.
Initial treatment involves the application of ice, taping, taking painkillers and avoiding activities that aggravate the pain. Wearing a tennis elbow brace can help to protect the tendon. Your management will be progressed as you go through various stages of recovery.
If you are suffering from such symptoms, call us for an appointment.
You will have a thorough assessment to ensure that your pain is not arising from the neck, thoracic spine or from a rib ring dysfunction.
Regular episodes of vertigo (a sensation of whirling and loss of balance – with or without headache or nausea), often leads to a diagnosis of Vestibular Migraine (VM), though it usually takes some time to come to this conclusion, because Vestibular Migraine is only diagnosed after all other possibilities have been ruled out. This is the nature of Vestibular Migraine; inviting mystery and controversy.
The Vestibular System is responsible for our i) sense of balance and ii) awareness of where we are in relation to our surroundings and then iii) coordinating the two.
The cause of VM is unknown, although, despite the logical assumption that a disorder of the Vestibular System is responsible, research does not support this, but suggests that the Brainstem is involved.
This not surprising given that there is widespread agreement that the underlying disorder in Migraine is a sensitised Brainstem. The possibility that the Brainstem is sensitised in VM is supported by research demonstrating significant improvement in dizziness and motion sickness in migraineurs after taking a ‘triptan’ (the triptans are specific anti-migraine medication which prevents migraine by temporarily DE-sensitising the Brainstem).
Current treatment of VM is problematic; there is no single, preferred preventive medication. Indeed, pharmaceutical management for both acute episodes and prevention is a process of ‘trial and error’, relying heavily on clinical experience.
Vestibular Migraine episodes are often provoked by head movements. For some, episodes are triggered by moving visual activity such as traffic or movies. Patients are often advised to avoid triggers, however, motion is a part of life; avoiding movement is virtually impossible and an unacceptable option. Furthermore, we are surrounded visual activity!
The assumption that a disorder of the Vestibular System is responsible for VM often leads to treating the Vestibular System – why? Research shows that the Vestibular System in VM is normal.
Research suggests that the vestibular system is normal in VM; that the Brainstem in VM is sensitised and that neck disorders can sensitise the Brainstem, a disorder of the neck could be responsible for VM… it seems logical that a skilled examination of the neck occurs when investigating VM.
Clinical experience has identified signs and symptoms suggesting that a neck disorder is responsible and these are:
Examination of the upper cervical spine could identify the reason for sensitisation of the Brainstem in VM and these disorders can be treated successfully, lessening the impact of, or preventing, VM. This examination is relatively easy by those skilled and experienced in the Watson Headacheâ Approach.
For further information please call Proactive Physiotherapy 40536222
The spine is made up of the following structures:
Bones(vertebrae), ligaments, muscles, tendons, discs, and cartilage.
Inside the spine we have the spinal cord, a part of the central nervous system, its membranes and spinal fluid. So, the spine functions as a protector and container of the spinal column.
Our discs dry out and provide fewer vertebrae cushioning. They also become more vulnerable to herniation.
The little cushions or discs in the spine, that functions mainly as shock absorbers, gets less pliable and more rigid. This can lead to herniation, which can lead to the gel-like fluid in the centre of the disc pushing out (a bulging disc / “slipped disc”). This can then, subsequently, put pressure on a nerve root resulting in sciatica.
The ligaments and muscles in our spine become less flexible.
As we get older, we get stiffer. Flexibility and elasticity are lost due to old injuries, wear and tear and normal physiological ageing processes.
Our spine joints lose fluid and cartilage, contributing to spinal osteoarthritis.
This may also include the deposits of small pieces of bone inside the joints, called osteophytes. This can be extremely painful because it changes the joint congruence.
Our vertebrae lose mineral density and become thinner.
As we age our bone density decreases. From the age of 25 we lose bone density according to various sources.
We need to take care of our spines – we just have this one.
Contact us for an appointment to let us teach you how to take care of your spine.
If you’re trying to find relief from jaw problems and pain, physiotherapy for jaw pain can help. Problems with the temporomandibular joint (TMJ) can be frustrating, causing symptoms such as pain, headaches and restrictive jaw movement.
What is the Temporomandibular Joint?
The temporomandibular joints (TMJ) are the most frequently used joints in the body. They are responsible for assisting with eating, talking, and facial expressions. Disorders to the TMJ often involve at least one of the following structures:
Symptoms of TMJ Disorders
What are the Causes of TMJ Disorders?
Problems with the TMJ are considered a multifaceted musculoskeletal disorder. Some of the common causes include:
Diagnosing Temporomandibular Disorders
Temporomandibular joint disorders can be diagnosed by an appropriately experienced physiotherapist. Other professionals who can assist include your dentist or oral medicine specialist. Further testing may be required, such as an X-ray, MRI or a CT scan to access the severity of your condition.
Physio for TMJ pain will include an assessment to evaluate your muscle length and tension, jaw range of motion and your TMJ movement patterns. This helps to identify whether your TMJ disorder is due to an opening or closing problem.
TMJ opening disorders:
TMJ closing disorders:
Treatment for TMJ Disorders
After your initial assessment, your physiotherapist experienced in jaw disorders will determine the appropriate treatment required to manage pain and any contributing factors. TMJ physiotherapy may include:
If your TMJ disorder is caused by teeth grinding, clenching or stress, your physiotherapist may work in conjunction with your dentist. This can be very effective in reducing teeth clenching or grinding and reduce associated jaw pain.
Until you have begun treatment for your TMJ disorder it is recommended to avoid anything that may aggravate your condition where possible, such as:
TMJ conditions often differ from person to person so it’s always best to book an appointment with a qualified and suitably experienced physiotherapist to assess your condition. Physiotherapy for jaw pain is an effective way to identify if other structures are involved, provide relief from pain and deal with any underlying issues which may be causing the problem.
Your physio can use a range of techniques including exercises, massage, jaw mobility techniques and dry needling to design a treatment specific for your condition. To find out more about TMJ disorders and how you can find relief from pain, contact proactive physiotherapy Physio for assessment and advice. Ph 40536222

