As
healthcare professionals we all deal with patients with chronic pain every day.
According to the Australian Institute of Health and Welfare, 1 in 5 Australians
over the age of 45 suffers from chronic pain. In my practice as a physio, I see
young people also suffering from chronic pain on a daily basis.
Chronic pain can result from injury, surgery,
musculoskeletal conditions such as arthritis, or other medical conditions such
as cancer, endometriosis, or migraines. The term “chronic pain” refers to pain,
persisting longer than 3 months from different diagnoses and epidemiology.
Pain that is acute, or short-term, is a response to damaged
tissue and usually disappears once the tissue has healed.
Chronic pain is much more complex!
Consider the Biopsychosocial model of chronic pain:
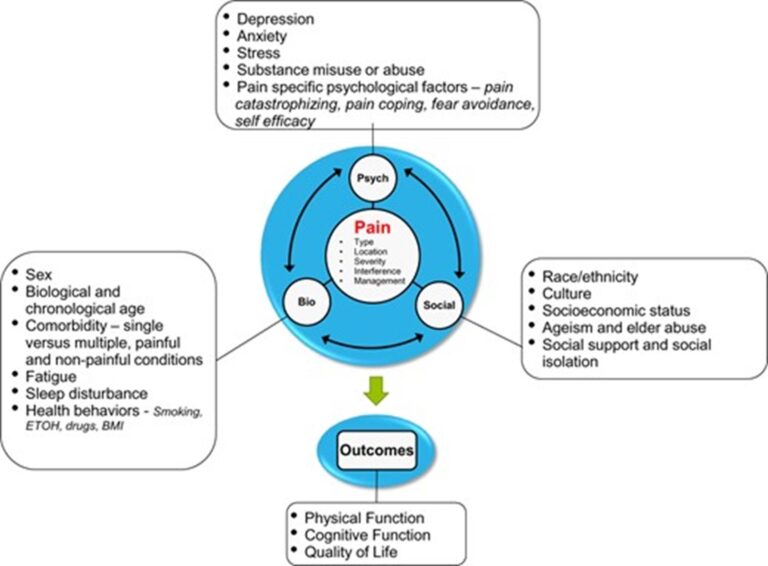
Image source: https://www.physio-pedia.com/Biopsychosocial_Mode
So, chronic pain may result from damage to body tissue from an acute or chronic condition.
But changes in the nerves or nervous system that result in the nerves continuing to signal pain after the original condition has healed (Painaustralia 2019a).
There also may be no apparent physical cause (Treede et al. 2015; Painaustralia 2019a).
Thus, attitudes towards pain and biological changes in the perception of pain may influence the experience of pain. (Molton & Terrill 2014).
There has been many studies and research to try to understand people’s experience of pain. One thing is for certain: Pain and the experience of pain is subjective. For instance, according to Professor Lorimer Moseley, of the USA in Adelaide, the more pain we feel the less life threatening it is. Why is this?
However, people suffering from chronic/persistent pain do have a lower life expectancy: It can disrupt nearly all aspects of someone’s life – beyond physical pain, it can impede their ability to work and participate in social and other activities like they used to. It impacts their relationships and cause feelings of isolation, frustration, and anxiety. Recently, Australian researchers have found that there are actual physical alterations happening in a patient’s brain that likely leads to negative changes in their personality.
Chronic pain itself is not life-threatening, but it leads to higher rates of depression, suicide, and opioid use.
What can we do about it?
As physiotherapists, we have many ways of trying to understand a person’s level of perceived pain, which is especially important for us to know if and how our treatment made a difference.
How can we address the changes in the nerves or nervous system, attitudes towards pain and perceived pain?
By combining an active and passive approach to meet the patient where they are at.
An active approach:
1) Empower the patient to understand their condition.
2) Provide education regarding chronic pain.
3) An exercise program that is gentle, gradually challenging fear and enhancing a sense of achievement.
4) Create an understanding, acceptive space to promote confidence.
5) Home exercises to promote self-management.
6) Self-management techniques to cope with setbacks or flare-ups.
7) Adopt a coaching role, assisting the patient to problem solve, rather than a traditional treatment plan.
A passive approach:
1) Hands-on modalities, including different massage techniques, joint mobilisations, myofascial release, and craniosacral therapy.
2) Electrotherapeutic modalities and cold/heat therapy and vibrations.
3) Acupuncture/ Dry Needling
In my experience, a combination of an active and passive approach is more appropriate and most useful.
To summarise:
An image to explain chronic pain:
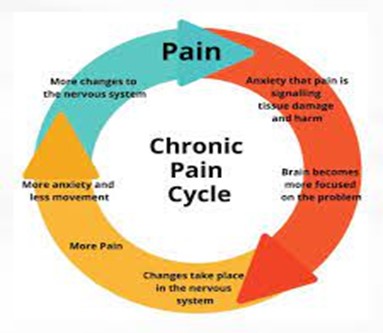
Our role as allied health professionals is to intercede into
this pain cycle and interrupt it. As we know, each person’s pain – experience
and perception are different.
So, we need to work with what the patient allows us to work
with. We need to do this with the patient, not “to” the chronic pain patient.
We need to have compassion, create trust, and provide
excellent care.
Resources:
www.aihw.gov.au
https://www.iasp-pain.org/publications/relief-news/article/pain-revolution-lorimer-moseley
https://www.healthdirect.gov.au/chronic-pain
https://www.adelaide.edu.au/painresearch
https://my.clevelandclinic.org/health/diseases