Pregnancy is a beautiful time of life full of lots of joy and excitement, but the female body will go through immense changes and pressures on different parts of the body. The pelvis area will come under tremendous strain during the pregnancy and will need treatment during pregnancy and after to remain in optimum health.
What is Pelvic Girdle Pain?
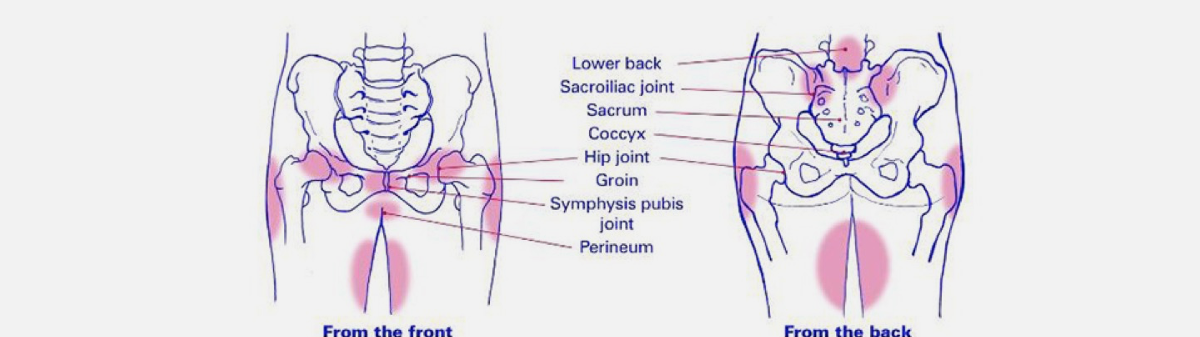
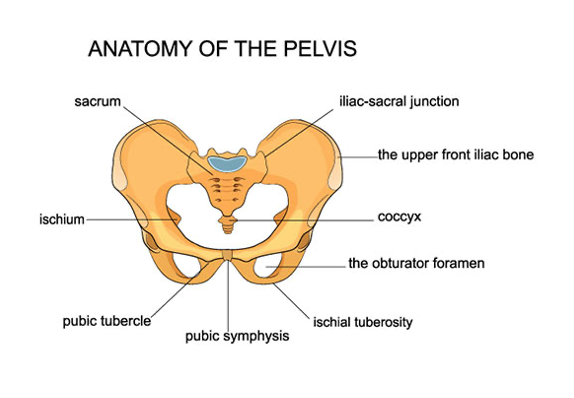
Pelvic Girdle Pain (or PGP) refers to pain around the pelvis, usually focusing on your two sacroiliac joints: the groin and your pubic symphysis.
The pain can often also be located down your thighs and in the lower back.
Often the most common symptoms of PGP associated with pain are caused by:
- Single legged activities, even as simple as walking or;
- Walking upstairs
- Rolling over in bed
- Getting in and out of the car
If you have PGP, your endurance capacity for standing, walking and sitting is decreased.
PGP can occur for several reasons:
- Trauma
- Injury
- Arthritis
- Rapid weight gain
- High BMI
- Weak pelvic floor muscles
PGP occurs most commonly in pregnant women. It’s so common that 25 per cent of pregnant women will suffer from some PGP through pregnancy. We call this pregnancy-related PGP.
As many as 50 per cent of women experience PGP during pregnancy. Happily, 90 per cent of women recover from PGP within 12 months of having their baby.
How to treat and manage PGP during pregnancy
There are two parts to treating PGP during pregnancy:
1. Treating the symptoms
As the belly expands and weight increases quickly, it can result in the pelvic joints becoming swollen and inflamed. Here’s a couple of ways to decrease inflammation.
- Ice the joints to settle the inflammation – Ice applied to the back and front of the pelvis for 20 minutes at a time.
- Rest the joints initially – Start by getting your body weight off the joints as much as possible. This means sitting or lying down when you can.
- Light exercise – It’s essential to rest the joints in the initial period but start specific exercises prescribed by your physiotherapist. This is important as the muscles need to get stronger, not weaker, progressively.
2. Treating the cause
Even if you were fit and active before pregnancy, never has your body experienced the effect pregnancy has on the biomechanics of your body.
For your joints to be well controlled, you must develop good awareness and control of your core muscles. Core muscles also help strengthen the back and trunk.
Your physiotherapist may initially prescribe a period of rest to settle your pain. However, it is vital to keep your muscles strong, so guided exercise should be undertaken after this initial rest. The main types of exercise that are important to address are specific stabilisation (movement control) exercises and cardio exercise (higher intensity exercise). Your physiotherapist will explain which form of each activity is appropriate for you. This is highly individual.
There are two types of exercise you’ll mostly likely be prescribed to undertake;
1. Cardio exercise
Some of the Cardio exercises you might be prescribed to do are:
Walking: Some people will be told to walk more or less depending on their condition.
Swimming: Swimming and water aerobics can work very well during pregnancy as the water takes away the pressure and weight of the tummy off the pelvis.
Cycling: a stationary bike is an excellent way to exercise if you can control your pelvic motion well. This involves having the correct seat height and handlebars set higher than you may typically be used to, to accommodate your growing baby.
2. Movement control exercise and aids
When your physiotherapist assesses you, they will determine which muscles you need to focus on. They can then decide which set of exercises will help your specific case.
Some control exercises might include:
- Squats
- Pelvic tilts
- Bridges
- Posture techniques
Some pelvic support aids may also be added to you therapy. These could be:
A pelvic support belt – can help improve movement control. However, make sure the belt has been recommended or fitted by your physiotherapist as you need one that supports you the correct way.
Tubigrip – is an elastic tubular bandage that can be fitted to wear around the tummy to aid your lower back and tummy muscles.
Spike balls – these can aid self-massage.
Once you have had your baby, your physiotherapist will be able to work with you on the therapy needed for PGP post-delivery, including rehabilitation.
Proactive Physiotherapy can help you with any of your pre and post-pregnancy pelvic issues. Contact us to organize your confidential appointment with one of our physiotherapists to get you back on track.